How Five States are Fighting Back against the Opioid Epidemic
The opioid crisis in America has left no one untouched. It has ravaged all demographics and regions, leaving no stone unturned.
The opioid crisis in America has left no one untouched. It has ravaged all demographics and regions, leaving no stone unturned. From high school students, to business executives, mothers, fathers, and friends, everyone has been impacted in some way by the epidemic that has swept across the nation. With overdose death rates climbing higher and higher each year, and resources to help those that are struggling becoming exhausted, the entire country has been left to answer the question “What do we do?” From devastated parents to politicians, everyone is searching for a solution. Lawsuits have been filed against pharmaceutical companies, insurance companies have begun to crack down on prescription practices, and law enforcement agencies have changed their policies in regards to dealing with addicted individuals. Opiate detox programs are in place, but not everyone wants to get help. As the pressure mounts from citizens who have been effected, governments too are changing their legislation. Below are five states that have begun fighting back in the battle against addiction.
- New Jersey- According to NJTV, the state has an overdose rate that is 3x the national average. A new program, NJ CARES (the office of the New Jersey Coordinator for Addiction Response and Enforcement Strategies) has been launched within the state’s department of Law and Public Safety, overseeing opioid response teams. The teams are comprised of law enforcement, licensed therapists and first responders that are available 24/7. Additionally, hospitals throughout the state have employed overdose specialists, often recovering addicts themselves, who meet patients’ bedside within one hour of being admitted to an emergency room after being administered an opioid reversal medication (Narcan). These specialists offer support and guidance, and help addicts find treatment. Former Governor Chris Christie signed a bill in 2015 mandating that sober housing be available to students at state colleges, and mandated that non-violent drug offenders receive inpatient addiction treatment instead of incarceration. More than $100 million has been allocated for treatment funding throughout the state.
- Vermont- Vermont declared the opioid crisis a state of emergency back in 2017, and is now considered to be a national leader in regards to program implementation. Efforts have been made to increase access to MAT (Medication Assisted Therapy), and a new model for treating addicted individuals has been implemented (it is known as “the hub and spoke model”). The hub is centered on an approach known as “multi-disciplinary, step down level of care” in the addiction treatment industry. It begins with intensive treatment, which includes daily visits to a clinic (usually for MAT) and treatment referrals, and over time decreases to weekly or monthly care at an outpatient facility as a patient becomes stabilized. The key to this program’s success is that The Affordable Care Act has made funding possible. Residents of Vermont no longer need pricey, top tier insurance to gain access to treatment services. The program is paid for almost entirely by Medicaid and Obama Care policies. It has been so successful that other states throughout the country have begun adopting the model. The hub and spoke system serves more than 8,000 people throughout the state, and in some areas has almost completely eradicated the wait lists for treatment beds.
- Georgia- An A&E Intervention Special, The Heroin Triangle, documents “ground zero” of the opioid epidemic in Georgia’s affluent suburbs. The triangle encompasses four counties where overdose rates have skyrocketed in the past six years- increasing by 3,844%, according to WXIA-TV. Earlier this year the state unanimously approved legislation to establish a state director of substance abuse, addiction, and related disorders to address the crisis. $11.7 million in federal grants has been allocated to the state of Georgia towards the fight against the epidemic.
- Washington State- The attorney state general estimated that two people die each day in Washington as a result of opioid overdose, and more than $9 billion was spent throughout the state on costs relating to the crisis in 2016 alone. To help combat the epidemic Washington has adopted the same hub and spoke model that started in Vermont, and state Medicaid covers the entire cost of Medication Assisted Treatment for patients (private insurers in the state must cover the services as well). It is through this program that residents in need are gaining access to therapy and treatment resources, and the state is working hard to educate people on the fact that addiction is a treatable medical condition opposed to a behavioral issue. Washington is one of the twelve states in the country with the highest ratio of MAT providers relative to how many drug fatalities occur each year.
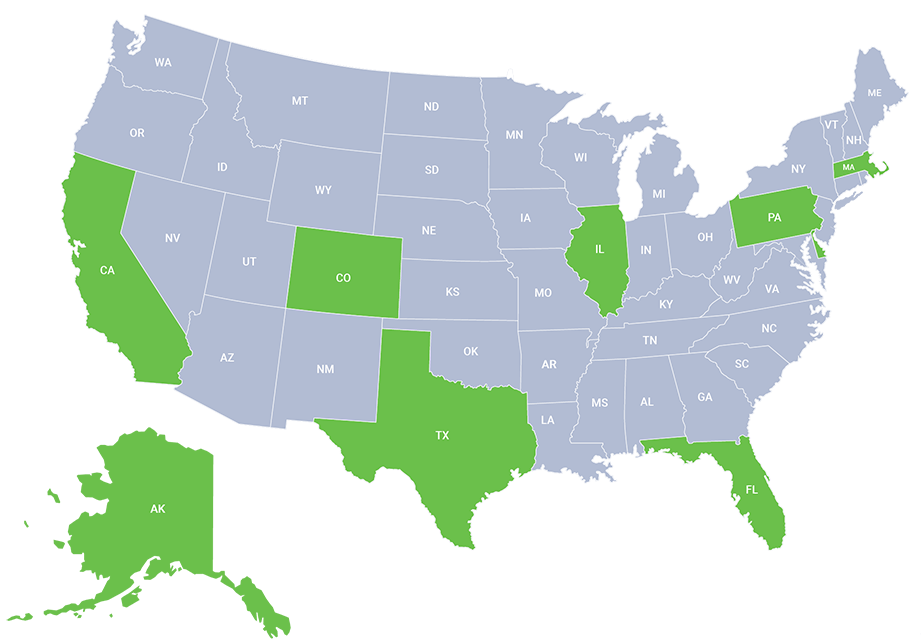
- Massachusetts- According to the state of Massachusetts’ government website, the rate of fatal overdoses in the region is more than double the national average, with eastern parts of the state being hit the hardest. In response, the governor’s office has put together a “Working Group on Opioids” that regularly develops and updates an action plan to address the state emergency. Communities have launched the “Angel Program” focused on helping those who are struggling to find treatment and recovery, rather than face punitive action. A main component of the program is that any addict can present at a police station asking for help, and they will be offered a bed in a treatment program without facing any legal repercussions. The program has been effective- more than 95% of those who showed up were successfully placed in beds, according to the New England Journal of Medicine. Individuals who commit to the program are given an “angel,” or mentor of sorts to guide them through each step of the recovery process, maintaining contact beyond that first interaction. Ten other states have followed this Massachusetts model, including Michigan, Connecticut, Ohio, Florida, Illinois, Maine, Missouri, New York, Pennsylvania and Vermont. In Mass., funding for the program comes by way of money seized in drug busts.
Getting into treatment is easy with our free insurance verification
"*" indicates required fields
While the fight against the opioid epidemic is far from over, many states have progressed from the “not in my neighborhood” mentality that was once so common. Citizens and politicians alike are demanding action, as their communities have been devastated by the death tolls resulting from opiate overdoses. The process seems to be by trial and error, as today’s public health emergency is one that has been unprecedented in the United States. With government bodies now working closely with residents in their home states, the gap is being bridged between idea and legislation. Although many questions regarding the solution to the opioid crisis remain unanswered, one thing is clear: Americans everywhere are searching for and demanding action; and the government has begun to respond.