Heroin addiction in veterans is a concerning trend on the rise. While many veterans would never have thought they’d be struggling with addiction, it happens all too often. According to the Veterans of Foreign Wars (VFW), the number of U.S. veterans with opioid addiction has doubled since 2002.1 Many who are serving or have served in the military struggle with substance abuse, and those who were exposed to combat also have co-occurring disorders, such as depression or post-traumatic stress disorder in addition to addiction. If you suspect that a veteran in your life is using heroin, we’re sharing some signs to look out for and treatment options that can help.
Questions about our Facilities or Programs?
Our admissions coordinators are available 24/7 to answer any questions you may have as you consider whether treatment at Banyan is right for you or your loved one.
Risk Factors of Heroin Abuse in Veterans
The most common risk factors of heroin abuse in veterans are mental illness and pain. Many veterans with substance abuse problems also have mental health disorders. The combination of an addiction and mental illness is otherwise referred to as a co-occurring disorder or dual diagnosis. These may include PTSD, traumatic brain injury (TBI), anxiety, and depression.
PTSD is especially common in veterans. These individuals are exposed to different types of trauma, including war zone deployment, training accidents, and military sexual assault (MSA), all of which can lead to PTSD. The prevalence of PTSD in veterans varies depending on their service era. While 11% to 20% of veterans who served in Operation Iraqi Freedom (OIF) and Operation Enduring Freedom (OEF) had PTSD in a given year, 12% who served in the Gulf War (Desert Storm) had PTSD in a given year.2
Returning to their families after experiencing the stress of deployment in war-torn regions and the trauma of combat creates additional challenges that veterans are often not equipped to handle. As a way of coping with the aftermath of their deployment and the sudden demands and changes in their new routine, veterans may turn to drugs and alcohol for comfort.
In addition to stress and mental illness, another contributing factor to heroin addiction in veterans is pain. 65% of U.S. veterans suffer from some type of pain, and 9.1% consider their pain to be severe.3 Pain is common in veterans who have experienced severe injuries often accompanied by PTSD and traumatic brain injury (TBI.) As a result, it’s become common practice to prescribe high-dose opioids to veterans to help them recover from combat-related injuries and cope with chronic pain.
Some common drugs prescribed to veterans include opioids (Lortab, Vicodin, OxyContin), benzos (Ativan, Valium, Xanax), and sedatives (Ambien, Lunesta). However, these veterans are often already struggling with other stressors, and prescribing them a highly addictive narcotic usually opens the floodgates for substance abuse.
Eventually, as the individual’s drug use becomes more severe, their prescribed doses may stop acting as they’re meant to due to increased tolerance. The more they enjoy the pain-relieving and euphoric side effects of opioids, the stronger their need for the drugs grows. Veterans who have reached this point and become addicted to their prescription drugs may find it easier and cheaper to switch to heroin.
Heroin Addiction Symptoms in Veterans
So what are some common symptoms of heroin addiction in veterans that you should look out for? It can be difficult to tell if a veteran is struggling with addiction, especially if they’re a high-functioning addict. Some typical signs of heroin addiction to look out for in veterans include:
- Sudden changes in behavior
- Mood swings
- Pinpoint pupils
- Slurred speech
- Disorientation and confusion
- Drowsiness
- Difficulty staying awake
- Extreme weight loss
- Hyper-awareness followed by drifting off
- Track marks on the arms, legs, or feet
- Abscesses or infections at injection points
The presence of heroin paraphernalia can also be a red flag for addiction. These may include burnt spoons, small plastic baggies with white powdery residue, cotton balls, bottle caps, and more.
Getting into treatment is easy with our free insurance verification
"*" indicates required fields
Heroin Addiction Treatment for Veterans
Veterans looking for heroin addiction treatment can come to our military rehab center for help. Our Military and Veterans in Recovery program is specifically designed to treat veterans and cater to their particular needs. We know that men and women who have served in the military have come face-to-face with trauma, combat, sexual assault, and more, and we wanted to create a program just for them.
Through the use of medically assisted detox and other veterans and military drug rehab programs, Banyan is able to give back to the strong servicemen and women who have fought for our country in a comfortable and judgment-free environment. If you or a loved one is a veteran struggling with addiction, reach out to us today.
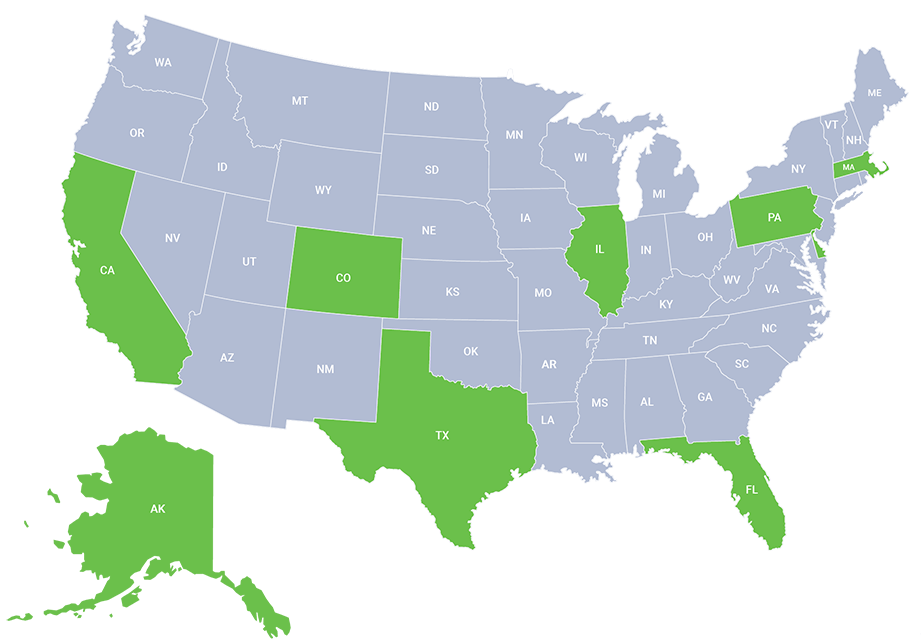
Call Banyan Treatment Centers at 888-280-4763 to learn how our nationwide military and veterans addiction treatment centers can help you.
Sources:
- VFW – VA’S Drug Abuse Stats Are Sobering
- US Department of Veterans Affairs - PTSD: National Center for PTSD
- National Library of Medicine - Severe Pain in Veterans: The Effect of Age and Sex, and Comparisons With the General Population
Related Reading: